Demo Topic: Diagnostic Pacing
The concept of electrophysiology was first recognised in the 1960’s, followed by diagnostic simulation in the 1970’s and finally RFA in the 1980’s (Boyle, 2002). This section explains the main protocols and their uses: to induce, to measure, or to terminate a tachycardia.
From this point forward it is assumed that all students are familiar with the common pacing terminology explained in Pacing 1 – Fundamentals (such as “S1”, burst, BPM conversion to milliseconds, etc).
6. Synchronizing pacing
During this course we have talked extensively about the importance of synchronizing pacing: having a good sensing signal, matching the pacing protocol with the type of synchronization and knowing the parameters related with synchronization of your cardiac stimulator.
Delay first S1
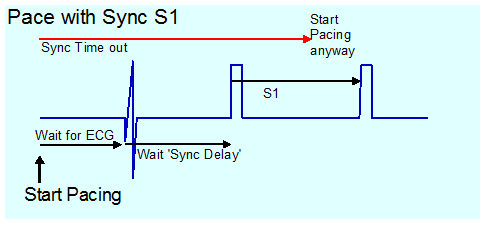
Delivering a S1 train without no synchronization may cause the first few S1 stimuli to not capture, delaying start of stimulation and adding a small risk of stimulating the heart in the vulnerable period causing VF.
Having this type of synchronization enabled and no ECG signal may hold stimulation off indefinitely. During an emergency, it has happened that urgent pacing was commenced, but no stimulation occurred due to this hold off. Advanced stimulators include a fail-safe timeout, so pacing starts after several; seconds regardless of ECG.
![]() Warning! Some stimulators have no timeout and in this mode, absence of ECG sensing leads to absence of pacing.
Warning! Some stimulators have no timeout and in this mode, absence of ECG sensing leads to absence of pacing.

Demand S1 pacing
This is similar to inhibited mode pacing used in “VVI” pacing. With pacing mode set to demand, S1 pacing will only be delivered if the S1 cycle length is shorter than the cycle length on the sensed channel.
This is not frequently needed. If mapping an AVRT pathway during tachycardia, breaking the tachycardia by ablating the pathway will result in sudden change of heart rate (from SVT to sinus), which will be accompanied by a large movement of the heart which will commonly displace the catheter). This results in a partially effective ablation, which results in a poor outcome as the pathway may be stunned but recover at a later time. Further mapping of a “stunned” pathway may not be possible.
If demand S1 pacing is used 20ms longer than the TCL, as soon as the pathway is interrupted, ventricular pacing is delivered slightly slower than the original tachycardia, with no significant movement of heart or catheter.
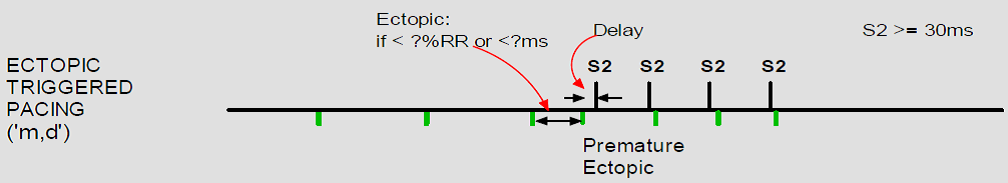
Some other use may be as well in VT Induction, for this S1 has to be adjusted for starting when ectopic beats occurs.
Another use could be during the ablation of AV Node. In this case it is required to start pacing automatically on AV block.