Demo Topic: Diagnostic Pacing
The concept of electrophysiology was first recognised in the 1960’s, followed by diagnostic simulation in the 1970’s and finally RFA in the 1980’s (Boyle, 2002). This section explains the main protocols and their uses: to induce, to measure, or to terminate a tachycardia.
From this point forward it is assumed that all students are familiar with the common pacing terminology explained in Pacing 1 – Fundamentals (such as “S1”, burst, BPM conversion to milliseconds, etc).
5. Specialized pacing protocols
Zipes test: AVJRT versus AVNRT
Ablation in the slow pathway area commonly results in junctional beats, and these are markers of effective ablation. However, these may be persistent following the end of ablation, or may be triggered by the use of isoprenaline. This can result in a tachycardia which is similar in appearance to the initial AVNRT, but is in fact an automatic junctional tachycardia (at 130-140bpm, for which no further treatment is required).
Two diagnostic tests can be used to differentiate the two tachycardias.
The first has to be described [Ref 1] uses atrial extra stimuli delivered during the tachycardia, scanned progressively earlier over a range of intervals, until His coincident, and then earlier. (This has been explained previously in the Section “Arrhythmia Entrainment”)
If a His coincident atrial extra stimulus perturbs the timing of the following His signal, then the diagnosis is AVNRT as the junction could not have been affected (his coincident / refractory).
If the atrial extra results in advancement of the immediate His, and the tachycardia continues, the diagnosis is Junctional Tachycardia (in AVNRT the retrograde fast pathway would have been blocked causing termination).
The second test is called His-synchronous PVC (or Zipes test). During a tachycardia a synchronized ventricle extra stimuli will be delivered. The timing of the extrastimulus that is delivered is critical, and should be synchronized with the tachycardia. Single extra beats are introduced to capture the right ventricle, intended to occur at exactly the same time as the His signal seen on the His catheter.
By `scanning` earlier with successive 10ms decrements, the extra is delivered 20-30ms earlier than the observed His signal, then the earliest atrial signal following the PVC is monitored for any 'perturbation' in timing.
In AVNRT the ventricular extra stimulus should never alter the atrial activation time as the route up to the atrium is blocked by the His which has been depolarized, in contrast to AVRT where there is another route up to the atrium [Ref 2].

Differential atrial pacing after Flutter ablation
A very good example of differential pacing is performed after an atrial flutter ablation to demonstrate completeness of block of re-entrant pathway. It involves pacing at different distances away from the ablation line along the Cavo-tricuspid isthmus (CTI). The physician will observe if the activation of the other side of the ablation line has occurred across the ablation or by going around the atrium (slow conduction versus block).
Pacing is required from 4 different sites on the tricuspid annulus, and conduction times compared to ensure that the impulse does not travel through the CTI.
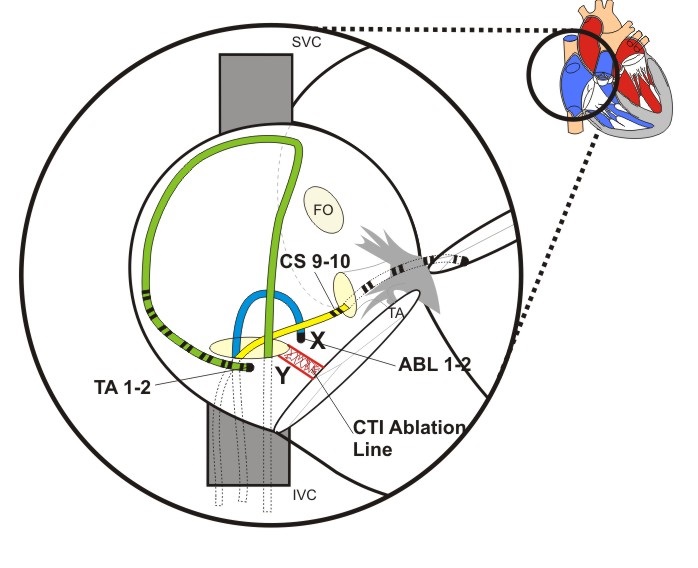
Figure above shows a view of the Right atrium with diagnostic catheter at the lateral RA wall, a CS and an ablation catheters. The Isthmus Ablation Line has been performed between the Inferior Vena Cava and the Tricuspid Annulus.
The exact procedure may be found accessing here:

Para-Hissian pacing
This test can reveal the existence of a concealed pathway, but it does not show that the pathway is part of a circuit, nor responsible for palpitations or tachycardia.
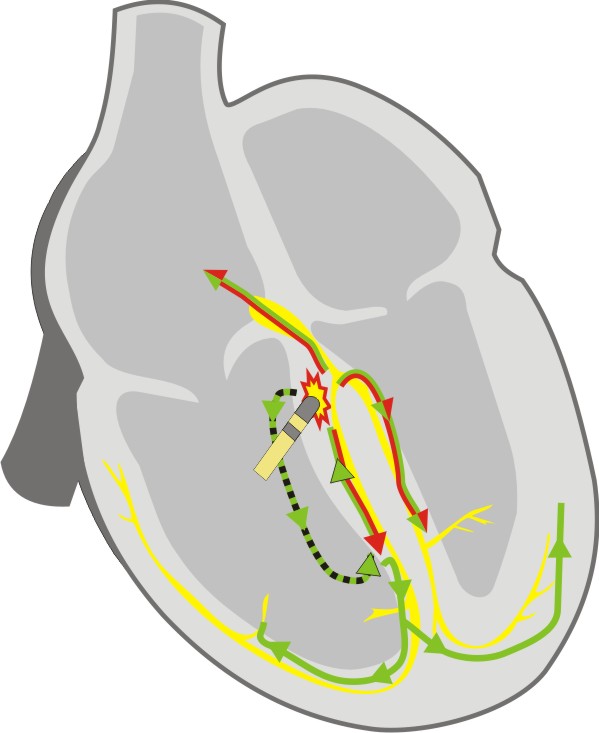
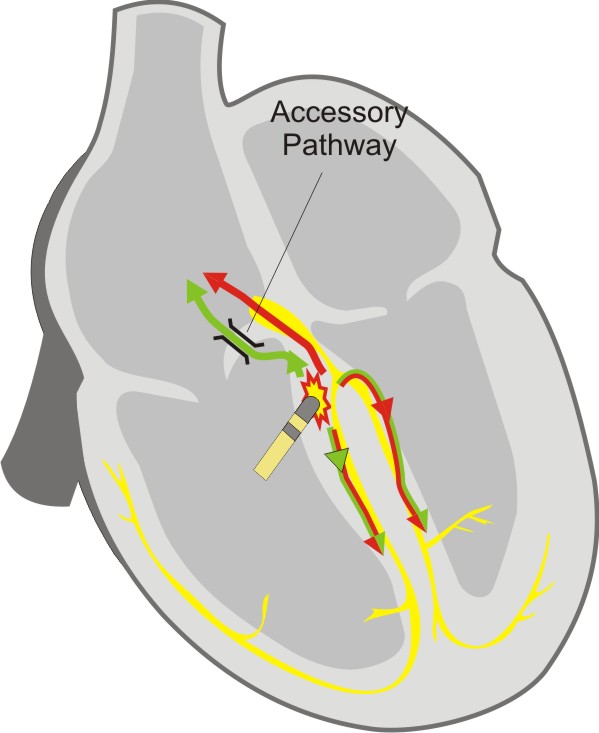
The test is always performed in sinus rhythm [Ref 3]. The His catheter is used for pacing from the distal electrodes. Pacing at maximum output aims to capture the His bundle. This results in a surface ECG which appears similar to the normal QRS (that means relatively narrow). The resultant atrial activation is observed (Stim-A time). The pacing output is then decreased until His bundle capture is lost, and the QRS becomes wider. The atrial activation is re-assessed.
Normal conduction results in a prolongation of the stim-A time with the transition from narrow complex capture to wide complex capture. Where there is no change in Stim-A time, a para‑hissian pathway is present. Ensure that direct atrial capture does not occur, as this is often seen when pacing from the His catheter.
|
|
Normal Physiology During His bundle capture the atrium is activated by direct conduction from His to AV node. After loss of His bundle capture, myocardial capture and conduction spreads down the interventricular septum to enter the Purkinje fibres, and travel back up the bundle branches to the His bundle and AV node. The increase in distance covered by the paced beat results in an increase in the Stim to Atrial activation time Red - Conduction Path with High Output pacing (Hisian capture) Green - Conduction path with Low output pacing (ventricular capture) |
|
|
Septal accessory pathway During His bundle capture, the atrium is activated via the accessory pathway, which appears similar to the AV node. After loss of His bundle capture denoted by widening of the QRS, the atrium continues to be activated by the accessory pathway, and the Stim to Atrial time remains unchanged as there has been no requirement of the Purkinje fibres or His bundle to excite the atrium. Red - Conduction Path with High Output pacing (Hissian capture) Green - Conduction path with Low output pacing (Ventricular capture) |
It is important that when pacing the His bundle at high output, that the atrium is not simultaneously captured.

Oesophageal pacing
Transesophageal atrial pacing is possible because of the proximity between the oesophagus and the posterior aspect of the atria. This technique is non-invasive, therefore there is no need to bring the patient to the cathlab, This method has been mainly tested in patients with a history of spontaneous supraventricular tachycardia (SVT).
Bipolar or unipolar recordings can be made, but obviously the strengh-duration curve of esophageal pacing is different than that of endocardial pacing. Acording to some studies, lowest thresholds can be reached at pulse widths between 10 and 20 msec and 5-15mA.
In order to minimize the patient discomfort, the studies have tried to use lower pacing thresholds using a bipolar electrode with wide interelectrode distance. [Ref 4]
In conclusion, using a rapid atrial pacing from the esophagus can be used to induce and terminate SVT for diagnostic or therapeutic purposes; and that esophageal pacing provides a convenient way to assess repeatedly the efficacy of long-term drug therapy and to screen patients for preexcitation syndromes. [Ref 5]
However, a few limitations to the technique have been found:
a) there is only one site of atrial pacing and recording,
b) there is no ventricular pacing and
c) sometimes atrial capture can be difficult to assess on the surface ECG during premature extrastimuli delivery.
References:(Ref 1) Padanilam BJ, Manfredi JA, Steinberg LA, Olson JA, Fogel RI, Prystowsky EN. Differentiating junctional tachycardia and atrioventricular node re-entry tachycardia based on response to atrial extrastimulus pacing. J Am Coll Cardiol 2008;52:1711-7.(Ref 2) Zipes DP, DeJoseph RL, Rothbaum DA. Unusual properties of accessory pathways. Circulation 1974;49:1200-11.(Ref 3) Hirao K, Otomo K, Wang X et al. Para-Hisian pacing. A new method for differentiating retrograde conduction over an accessory AV pathway from conduction over the AV node. Circulation 1996;94:1027-35.(Ref 4) Thierry Verbeet MD, José Castro MD, Pierre Decoodt MD. Transesophageal pacing : a versatile diagnostic and therapeutic tool. Department of Cardiology, University Hospital Brugmann, Brussels, Belgium.(Ref 5) J J Gallagher, W M Smith, C R Kerr, J Kasell, L Cook, M Reiter, R Sterba and M Harte. Esophageal pacing: a diagnostic and therapeutic tool.