Demo Topic: Diagnostic Pacing
The concept of electrophysiology was first recognised in the 1960’s, followed by diagnostic simulation in the 1970’s and finally RFA in the 1980’s (Boyle, 2002). This section explains the main protocols and their uses: to induce, to measure, or to terminate a tachycardia.
From this point forward it is assumed that all students are familiar with the common pacing terminology explained in Pacing 1 – Fundamentals (such as “S1”, burst, BPM conversion to milliseconds, etc).
3. Measuring tachycardias
Arrhythmia Entrainment
Entrainment is performed because the first returned beat of a tachycardia after entrainment can provide much diagnostic information.
Entrainment of an arrhythmia involves pacing during tachycardia, at a slightly faster cycle length. After pacing is stopped, the last few atrial signals are measured and assessed to ensure that they were accelerated to the paced rate. If they were not, then the tachycardia was not entrained, and the maneuver should be attempted again.
![]() If pacing caused tachycardia termination, then the PPI cannot be assessed, and the tachycardia should be re-induced in order to make a further attempt at entrainment.
If pacing caused tachycardia termination, then the PPI cannot be assessed, and the tachycardia should be re-induced in order to make a further attempt at entrainment.
If you have successfully entrained, then the first beat after you stop the pacing, will be identical in appearance to the intrinsic tachycardia and the same tachycardia (morphology and timing) will then continue as before pacing.
We inspect the first post pacing beat for the following:
- Post Pacing Interval, to tell us if the pacing catheter is in the arrhythmia circuit (and is therefore a good place to ablate). This applies to any re-entrant tachycardia such as VT, SVT and Flutter.
- The pattern of activation of first post pacing beat (E.g.: V-A-V or V-A-V-V, which tells us if SVT is re-entrant or atrial tachycardia.).
Post Pacing Interval (PPI)
Following the entrainment of an arrhythmia, the time taken for the next electrogram to be sensed on the pacing catheter is termed the post pacing interval.
This is used to identify location of the circuit.
The difference between the PPI and the TCL is an indication of the distance of the pacing catheter to the re-entrant circuit (6;7). The PPI must be > TCL (if not entrainment probably did not occur). If the PPI is within 30ms of the TCL, then the pacing catheter is thought to be inside (or very close to) the re-entrant circuit.
![]() To summarize:
To summarize:
-
-
-
- If PPI – TCL >= 0, there will be entrainment
- If PPI – TCL <= 30, the pacing catheter is very close to the circuit
-
-

Resetting
An arrhythmia can be reset by inserting a single stimulus into the excitable gap of a circuit. Entrainment described earlier is an example of repetitive resetting.
There are several conditions to reset a reentrant tachycardia:
- The stimulus must reach the circuit through the entry site or critical isthmus),
- Enter the excitable gap of the circuit (where tissue is excitable)
- Collide with the ongoing tachycardia wavefront
- And propagate through the tachycardia reentrant path (also called by some physician ‘critical isthmus’) to the exit of the circuit.
The exit of the resetting wave should be at an earlier than the tachycardia time (accelerate the tachycardia) and, in most of the cases, capture the tachycardia circuit at that pace.
![]() Resetting with Fusion: When resetting is successful and a change in the morphology of the tachycardia complex is observed on surface ECG or intracardiac electrograms, that is called “fusion”. In the electrograms can be observed the progressive advancement of the entrainment and how the pattern changes from the natural tachycardia complex to the stimulated tachycardia complex.
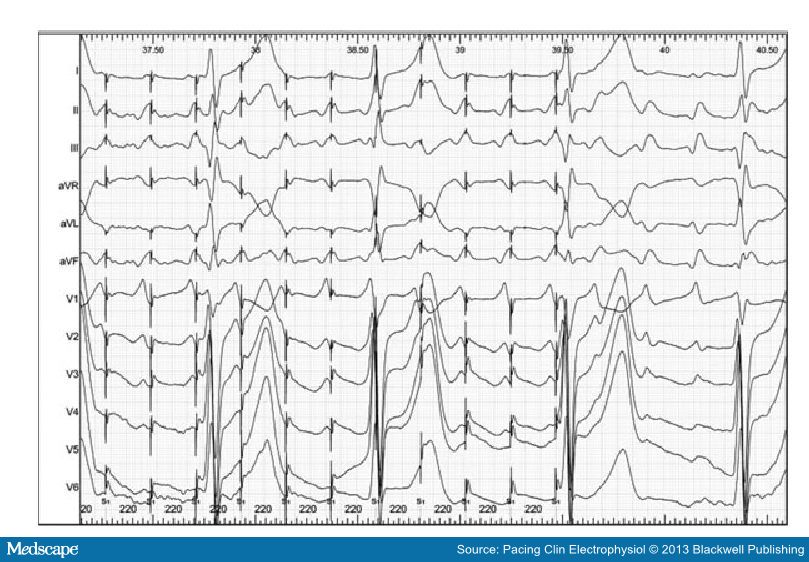
Resetting with Fusion: When resetting is successful and a change in the morphology of the tachycardia complex is observed on surface ECG or intracardiac electrograms, that is called “fusion”. In the electrograms can be observed the progressive advancement of the entrainment and how the pattern changes from the natural tachycardia complex to the stimulated tachycardia complex.
Below [Pic 1], we can see an example of entrainment with fucion in a 12 ECG electrogram.
Termination
Many times the termination of the tachycardia occurs during the attempts of entrainment.
Termination could be happen when the extrastimulus collides with the tachycardia impulse that is already in the reentrant circuit. Following the example of the previous section, the extrastimulus finds refractory period tissue antidromically and clashes orthodormically with the tachycardia wavefront terminating the arrhythmia.
If this is the case, some information can still be deduced based on how termination occurred.
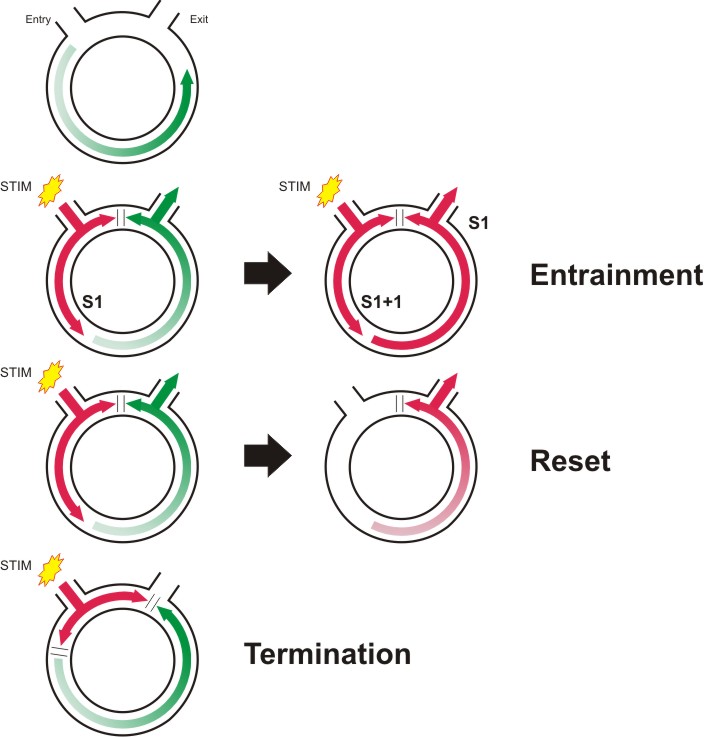
Above, you can find a little brief of the entrainment phenomenon.
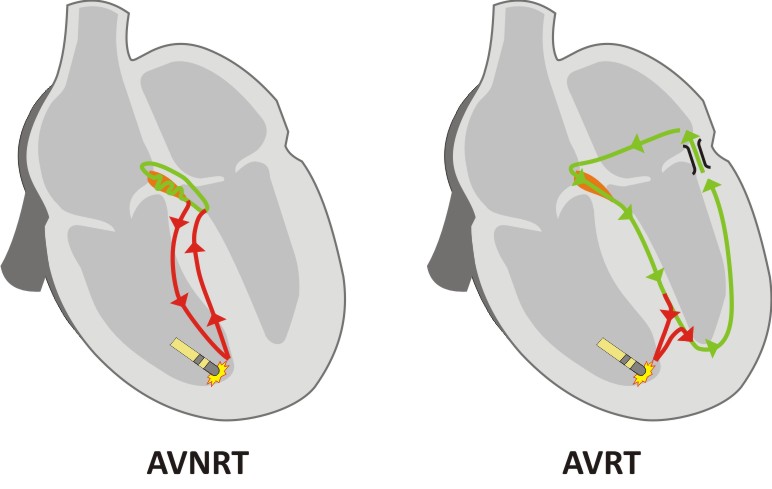
SVT, an illustrated example of Entrainment pacingUsing an S1 protocol, pacing is delivered to the RVA at 20ms faster than TCL. The PPI interval Then, if the tachycardia was successfully entrained, the time interval from the final S1 until the onset of the first sensed beat on the RVA is measured. This is the PPI. This value can be compared with the smaller value TCL. As shown in the figure on the right, the PPI is approximately equivalent to the TCL (green) PLUS the time taken for the pacing impulse to get from the RVA to the circuit and back again (red). We can see that the PPI minus TCL is much longer for AVNRT than for AVRT, as the circuit is further away. As a general rule, if the PPI is >115ms longer than the tachycardia cycle length, then the tachycardia is more likely to be AVNRT than AVRT. The TCL is determined by the green path, although the length of the path does not dictate the TCL, as the AVNRT path contains a slow AVN pathway which determines most of the cycle length. Above, graphic representation of AVNRT (left) and AVRT (right).
However, when entraining a tachycardia, the tachycardia must by definition be temporarily accelerated. This can lead to prolongation of conduction over the AVN due its decremental properties. Therefore in borderline cases, or where doubt exists, the corrected post pacing (cPPI) interval should be assessed. Here, the AH time prior to the entrainment is measured, and the AH time measured on the last beat of entrainment. Any increase in the value is subtracted from the measured PPI to give a cPPI. A cPPI-TCL of >110ms is highly suggestive of AVNRT.
The pattern of response The pattern of response following the last paced beat can also provide useful information. Following the final paced V signal, if the order of the following electrograms is “A-V”, then the diagnosis is either AVNRT or AVRT. If the order is “A-A-V”, then the diagnosis is atrial tachycardia.
The transition zone It is important to ensure that the first paced beat is synchronized to the tachycardia, and that ventricular pacing gradually fuses with the tachycardia. When this occurs, the timing of the first accelerated atrial electrogram may indicate the presence of a concealed accessory pathway. During the onset of entrainment, the surface ECG morphology gradually changes from the narrow complex tachycardia to that of a paced complex. The time over which this change takes place is termed the transition zone. [Ref 2] If the atrial electrogram accelerates from TCL to the paced rate during the transition zone, an accessory pathway must be present. Why? Because of fusion to have occurred, the pacing must have fused with impulses traveling down the His bundle. Therefore retrograde atrial acceleration must have occurred by another route. If atrial advancement occurs following the stabilization of a purely paced complex morphology (after transition zone), then advancement probably occurred over the retrograde AV node.
Termination When ventricular pacing terminates an SVT, the mechanism of termination can assist in diagnosis of the tachycardia. If the atrial rate was not affected by pacing, atrial tachycardia is excluded, as a premature atrial event would have been needed to terminate the SVT. An accessory pathway is also unlikely as the pathway would usually conduct from the V to the A. |
A more specific example of how to diagnose using entrainment? Click below.

Pace mapping
Pace mapping is a method of locating the source of ventricular activation, commonly used during ventricular tachycardia ablation. The technique requires a sample of the tachycardia or ectopic beat to have been recorded during the current clinical case, this will be the “template” (Note: old ECGs are not usually suitable due to variability in ECG electrode positioning).
With the recording “template” in a separate review window, the ablation catheter is paced using an S1 protocol at a low current. The resulting QRS complex is then compared to the template. If the resulting complex is identical to the template in all 12 leads, then the catheter is said to be at the origin of the clinical activation (breakout), but if not the ablation catheter is moved, and pacing repeated until an exact match is found.
If you are matching an ectopic, you can pace S1 quite slowly, say at 600ms, but if you are matching a VT, you need to pace at close to the VT cycle length, as pacing at slower rates can give subtly different morphology even when paced at the exact source.
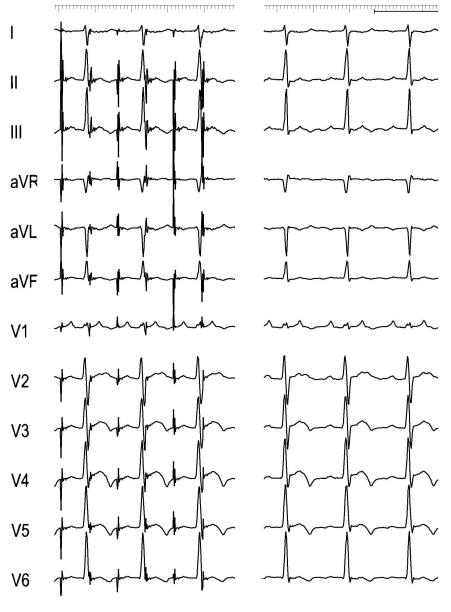
Example of atrial tachycardia pacemapping. Atrial pacing (right) to emulate the P waveform of the tachycardia (left) that it is used as a template. [Pic 2]