Demo Topic: Diagnostic Pacing
The concept of electrophysiology was first recognised in the 1960’s, followed by diagnostic simulation in the 1970’s and finally RFA in the 1980’s (Boyle, 2002). This section explains the main protocols and their uses: to induce, to measure, or to terminate a tachycardia.
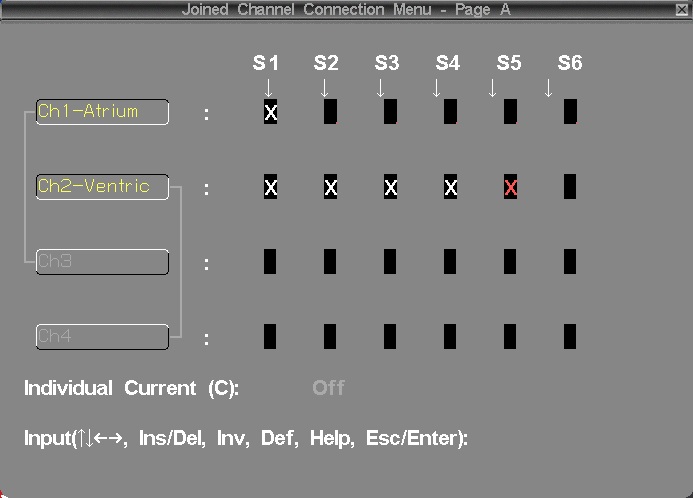
From this point forward it is assumed that all students are familiar with the common pacing terminology explained in Pacing 1 – Fundamentals (such as “S1”, burst, BPM conversion to milliseconds, etc).
2. Arryhthmia induction protocols
The induction of a tachycardia is in most cases the principal goal of pacing. The success of the induction depends on many factors such as: the stimulation location, the patient status, and of course, the mechanism of the tachycardia activation.
Rapid Burst pacing
Burst pacing can be used to trigger either re-entrant or focal triggered arrhythmias. When using Burst Pacing, it is recommended to deliver approx. 5-10 seconds of pacing at a time. The arrhythmia can be started at any point in the burst.
As arrhythmia induction using this method is based on probability, multiple attempts at varying cycle lengths are often required. For example, narrow complex tachycardias are typically induced by pacing slightly slower than the AV wenckebach rate, which is variable typically between 450 to 300ms. Atrial flutter is induced at faster rates between 300-220ms.
Inducing AF, for example in assessing WPW conduction, may be done with much faster pacing rates. Ensure that pacing is into the Atrium, as pacing rates faster than 200ms applied accidentally to the ventricle may cause VF.

![]() Warning!! Look carefully at ECG and make sure you see a sinus beat before restarting next burst pace. This is to make sure, in case you did succeed to induce the arrhythmia, that you don’t accidentally overdrive pace.
Warning!! Look carefully at ECG and make sure you see a sinus beat before restarting next burst pace. This is to make sure, in case you did succeed to induce the arrhythmia, that you don’t accidentally overdrive pace.
A common method of SVT induction is Pace at S1 just above Wenckebach rate. This method causes delay in the AV node, which allows retrograde pathway recovery, and re-entry. Select an atrial pacing catheter and use deliver S1 pacing at 10-30 longer than the AV Wenckebach cycle length.
If attempting to induce SVT, changing from HRA to CS catheter, which is closer to the re-entrant pathway may facilitate induction of arrhythmia. What could happen?

Single and multiple extra stimulus
This method of induction uses a single extra-stimulus to induce (usually) an SVT or a re-entrant tachycardia. The extra-stimulus may be placed after a number of sensed beats, but is usually placed after a paced train of eight (8) S1 stimuli, as this provides the most reproducible conduction characteristics.
The 8 beat S1 train is used to regulate the subsequent refractory period, or single timed extras can be delivered alone following a sinus beat. This is the most physiological method of induction as it mimics a single ectopic which is what triggers arrhythmia in most patients. But as with clinical arrhythmias, induction is less predictable.

Short-long-short stimulation
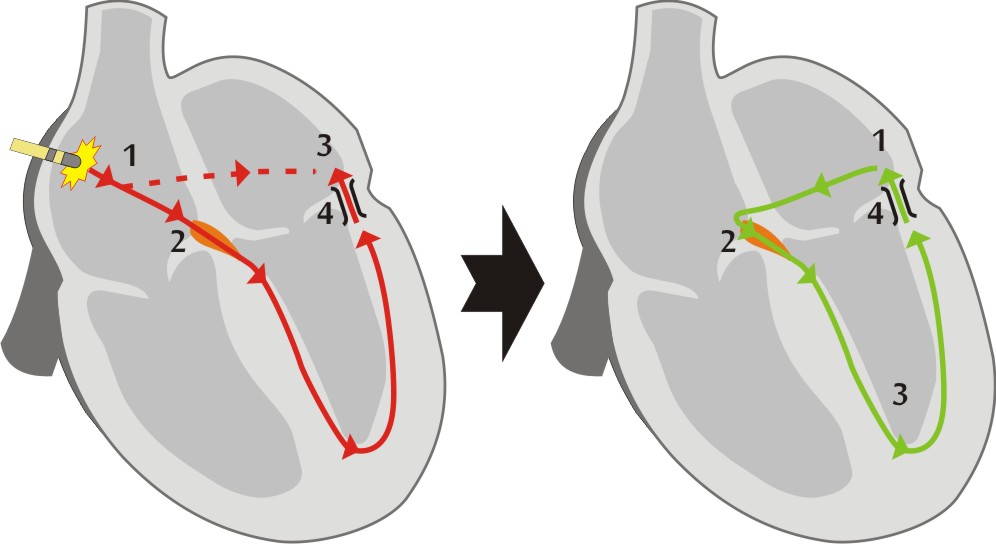
The induction of re-entrant arrhythmias requires that impulses travel round a circuit in one direction. In order to promote this, pacing aims to induce 'uni-directional' block, by maximizing the differences in conduction properties between the normal heart and a "pathway". The conduction velocity of an impulse in the myocardium is dependent upon the cycle length of the previous beat. Short-long-short stimulation uses a long coupling interval to lengthen the refractory period of myocardial tissue, making it more likely to block with the next short coupled extra which can conduct slowly into scar promoting re-entry.

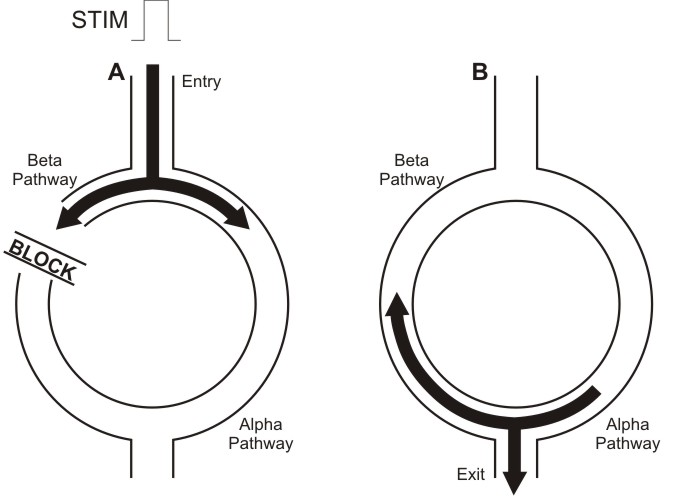
In the image above, we can a schematic representation of a re-entrant arrhythmia induction with extrastimulus. In diagram A, the pulse conducting through the Alpha pathway is blocked (in refractory period) meanwhile continues traveling through the Beta pathway. Later, in diagram B, when that pulse reaches again the Alpha pathway, this pathway has recovered so propagates the stimulus and starts the tachycardia.
Programmed ventricular stimulation
Ventricular tachycardia is usually induced by pacing using programmed ventricular stimulation.
The usual pattern (or Wellens protocol) consists in use 2 basic drive S1 cycle lengths (600 & 400ms). Following the conditioning train of 8 S1 beats, S2 is introduced from 300ms and decreased in 10ms intervals until it reaches refractoriness. Its timing is then fixed at 20ms above this point and an s3 introduced at 300ms which is then reduced in 10ms intervals. Further extra stimuli are delivered down to 200ms, at which point they are fixed and another extra added until 4 or 5 extras are used. The extra stimuli enhance differences between normal myocardium (where they increase conduction velocities) and scar (where they cause decremental type slowing). These conditions are ideal for the induction of re-entrant VT.
Pacing trains generally have a 3 second pause between repeat trains. Train repetition should not be interrupted if possible to maintain uniform condition of the myocardium.

Most physicians use up to 4 extrastimuli. Use of only 3 extra-stimuli may decrease sensitivity of the protocol (fail to induce VT in an existing pathological tachycardia circuit). The use of more than 4 extra-stimuli may induce clinically irrelevant tachycardias, especially VF.
To learn how to deal with common problems using extrastimuli to stimulate the ventricle:

There are alternative, less commonly used protocols, which may be faster, such as Wellens and Morady protocols. Learn about them here:

Drug assisted arrhythmia induction
Many cardiac arrhythmias are sensitive to autonomic state or circulating adrenaline. The most common example of this is supra ventricular tachycardia, which often requires isoprenaline to be given before an arrhythmia can be sustained.
Isoprenaline can be given as bolus doses, or as an IV infusion. It elevates baseline heart rate and decreases refractory periods particularly in the AV node. Isoprenaline infusion is usually administered until the baseline heart rate is elevated to at least 120bpm, or the baseline rate has elevated by at least 25% of the resting value. Diagnostic testing may then be repeated, typically with requiring a faster S1 drive cycle of 400ms to pace the heart.
Patient should be observed closely during isoprenaline infusion, because this drug occasionally may cause a paradoxical vasovagal reflex response, resulting in a tachycardia with profound hypotension.
Atropine can be used in a similar manner to isoprenaline, but is seldom used due to its side effects, prolonged duration of action and lack of reversal agent. It blocks the action of the vagus nerve on the heart. If used together with propranolol, a beta blocker which inhibits the sympathetic autonomic system, the heart can be studied in the absence of external autonomic influences, but this is rarely done clinically.
Following pulmonary vein isolation ablation, pacing manoeuvres are used to confirm the loss of conduction both into and out of the vein. Where conduction block is thought to be temporary, or is unclear, the injection of Adenosine can be used to temporarily augment conduction across the partially effective ablation line, identifying segments of incomplete ablation, which can then be re-ablated to cause permanent block.